PCOD vs. PCOS in India: Symptoms, Core Differences, and Management
In India, if you ask about irregular periods or hormonal issues, the terms PCOD and PCOS are often used interchangeably, creating a cloud of confusion. With nearly one in five Indian women affected by these conditions, getting clear answers is essential for health and well-being. So, what is the core difference?
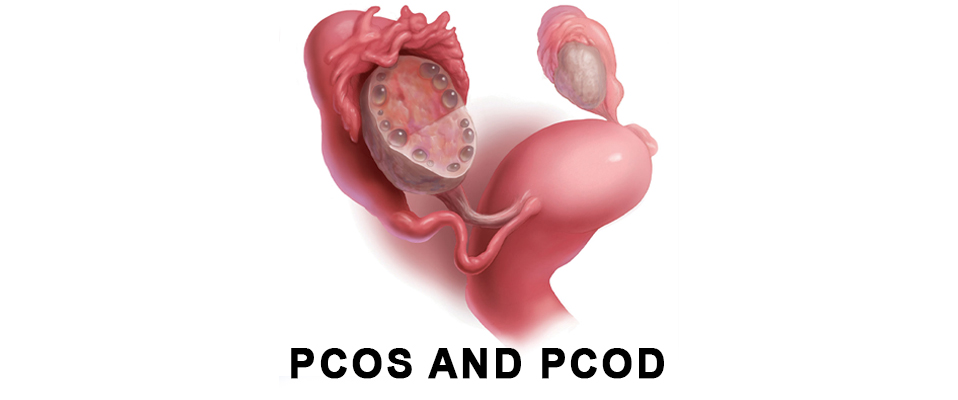
In simple terms, PCOD (Polycystic Ovarian Disease) is a common medical condition where the ovaries release immature eggs, leading to cysts and hormonal disturbances. In contrast, PCOS (Polycystic Ovary Syndrome) is a more severe and complex metabolic syndrome that affects the entire body's endocrine system, carrying risks of diabetes, heart disease, and infertility.
While PCOD is often manageable with lifestyle changes, PCOS demands a more comprehensive medical and lifestyle approach. This article will provide a detailed exploration of their symptoms, causes, and the most effective management strategies available in India, followed by answers to your most frequently asked questions.
PCOD vs. PCOS: Symptoms, Core Differences, and Management
Are you confused by the terms PCOD and PCOS? Do you hear them used interchangeably in conversations, on social media, and even in clinics? If so, you are certainly not alone. In India, where an estimated one in every five women grapples with these conditions, the lack of clarity can be a significant barrier to getting the right help. This widespread issue, a form of hormonal imbalance in women, affects everything from menstrual cycles and skin health to fertility and long-term well-being.
The journey to wellness begins with understanding. This comprehensive guide is designed to demystify the PCOD vs PCOS debate once and for all. We will delve into the core differences, explore the common and distinct symptoms, understand the root causes, and outline the most effective, holistic management strategies available right here in India. Our goal is to empower you with knowledge, so you can take control of your female reproductive health and work confidently with your healthcare provider.
First, What exactly is PCOD (Polycystic Ovarian Disease)?
Let’s start with the more common and generally milder of the two. PCOD, which stands for Polycystic Ovarian Disease, is primarily a medical condition, not a full-blown metabolic disease.
Imagine your ovaries as tiny, bustling factories that are supposed to produce and release one mature egg each month. In a woman with PCOD, these factories become slightly dysfunctional. They start producing a large number of immature or partially-mature eggs, which fail to be released. Over time, these unreleased eggs can turn into small fluid-filled sacs called cysts, causing the ovaries to become enlarged.
A hormonal imbalance drives this process, but it's often not as severe as what's seen in PCOS. While PCOD can cause frustrating symptoms like irregular periods and difficulty conceiving, its impact is largely confined to the reproductive system. It is a significant topic for menstrual health awareness in India because of its high prevalence, but it is considered a manageable condition that can often be corrected with targeted lifestyle changes.
What is PCOS (Polycystic Ovary Syndrome)?
Now, let's look at its more complex counterpart. PCOS, it's crucial to understand that PCOS (Polycystic Ovary Syndrome) is not a simple condition, but a complex syndrome that affects multiple systems throughout the body.. Specifically, it's a serious endocrine disorder with significant metabolic implications. This means it affects not only your reproductive system but your entire body's hormonal and metabolic functions.
The diagnosis for PCOS is more stringent. According to the globally accepted Rotterdam criteria, a woman must exhibit at least two of the following three signs to be diagnosed with PCOS:
- Irregular Ovulation (Oligo-ovulation or anovulation): This manifests as infrequent, irregular, or completely absent periods.
- High Androgen Levels (Hyperandrogenism): Androgens are often called "male hormones," though women produce them in small amounts. In PCOS, these levels are significantly elevated, leading to symptoms like excess facial hair, severe acne, and hair thinning on the scalp.
- Polycystic Ovaries on Ultrasound: The presence of multiple small ovarian cysts, similar to PCOD but often more numerous.
The critical distinction is the metabolic component. PCOS is intrinsically linked to insulin resistance, a condition where the body's cells don't respond properly to the hormone insulin. This makes PCOS a gateway to other serious health issues, solidifying its status as a significant women’s hormonal disorder.
The Core Differences: PCOD vs PCOS at a Glance
To make the distinction crystal clear, let's break down the key differences in a table. This will help you understand why knowing whether you have PCOD or PCOS is so important for your long-term health management.
|
Feature |
PCOD (Polycystic Ovarian Disease) |
PCOS (Polycystic Ovary Syndrome) |
|
Nature of Condition |
A medical condition caused by a hormonal imbalance. |
A complex endocrine disorder and metabolic syndrome. |
|
Severity |
Generally considered milder and more common. |
A more serious condition with systemic health implications. |
|
Prevalence |
Very common, affecting up to one-third of women globally. |
Less common than PCOD, but prevalence is rising in India. |
|
Hormonal Impact |
Mild hormonal imbalance, primarily affecting the reproductive cycle. |
Significant hormonal disruption, marked by high androgen levels and insulin resistance. |
|
Fertility Impact |
May cause temporary fertility issues, but women can often conceive with lifestyle changes or minimal medical help. Does PCOD cause infertility? Not always permanently. |
A significant cause of infertility due to chronic lack of ovulation. Conception often requires targeted medical intervention. |
|
Metabolic Risk |
Low to moderate long-term metabolic risk. |
High risk of developing Type 2 diabetes, high blood pressure, heart disease, and endometrial cancer. |
|
Core Cause |
Often linked to poor lifestyle, diet, and genetics. |
A combination of strong genetic predisposition, severe insulin resistance, and inflammation. |
|
Management |
Often managed effectively with diet and lifestyle changes alone. |
Requires a multi-pronged approach: aggressive lifestyle changes, medication, and regular health monitoring. |
So, PCOD vs PCOS, which is more dangerous? Based on the potential for long-term health complications like diabetes and heart disease, PCOS is considered the more serious and destructive of the two.
Unpacking the Symptoms: Are You Experiencing This?
While the underlying mechanisms differ, the outward symptoms can often overlap, which is a major source of confusion. Here’s a breakdown of common PCOD and PCOS symptoms in females, with notes on severity.
Menstrual Irregularities
- Irregular Periods: This is the hallmark symptom for both. It can mean periods that come too frequently, too far apart (e.g., more than 35 days), or are completely absent for months. This is typically more severe and persistent in PCOS.
- Heavy Bleeding (Menorrhagia): When you do get your period, it might be unusually heavy and painful.
Androgen-Related (Hyperandrogenism) Symptoms
- Hirsutism: Unwanted, coarse, dark hair growth on the face (chin, upper lip), chest, abdomen, and back. While it can occur in PCOD, it's a classic and more pronounced sign of PCOS.
- Severe Acne: Persistent, often painful cystic acne due to PCOS that doesn’t respond to typical treatments, common on the jawline, neck, and back.
- Hair Loss: Thinning hair on the scalp, sometimes resembling male baldness.
Metabolic Symptoms
- Weight Gain: A significant and frustrating symptom is unexplained weight gain in PCOD and PCOS, particularly around the abdomen. This is strongly linked to insulin resistance and is harder to manage in PCOS.
- Skin Darkening (Acanthosis Nigricans): Dark, velvety patches of skin, typically found in body folds like the back of the neck, underarms, and groin area. This is a direct sign of insulin resistance..
The Root Causes: Why Does This Happen to Indian Women?
What causes PCOD in Indian women? The answer is a complex interplay of genetics and environment, a combination that makes South Asian women particularly susceptible.
- Strong Genetic Predisposition: If your mother, sister, or aunt has PCOD or PCOS, your risk is significantly higher. South Asian genes are also linked to a higher predisposition for insulin resistance.
- Insulin Resistance: This is the metabolic villain at the heart of PCOS. In the Indian context, a diet traditionally high in refined carbohydrates (white rice, roti made from fine atta, sweets) and a genetic tendency towards central obesity (fat around the waist) makes insulin resistance a widespread problem.
- Chronic Inflammation: Research shows that women with PCOS often have a type of low-grade inflammation that stimulates the ovaries to produce more androgens, contributing to the cycle.
- Lifestyle Shifts in Modern India: The rapid urbanization across India has led to profound lifestyle changes. A more sedentary desk-bound life, increased consumption of processed and fast foods, and chronic stress are major environmental triggers that can unmask a genetic predisposition to PCOD and PCOS.
Diagnosis in India: Getting the Right Answers
If you are experiencing any of the symptoms mentioned, the first and most crucial step is to get a proper diagnosis. Self-diagnosing based on internet articles is not enough. You need to consult a healthcare professional, typically starting with a gynaecologist. Here’s what you can expect during the diagnostic process:
- Detailed Medical History: Your doctor will ask about your menstrual history, symptoms, and family history of PCOD/PCOS or diabetes.
- Physical Examination: This includes checking your weight, blood pressure, and looking for physical signs like acne and hirsutism.
- Blood Tests: This is non-negotiable. A hormone panel will check your levels of androgens, LH, FSH, and thyroid hormones. Your doctor will also order tests to check your blood sugar and insulin levels (Fasting Glucose, HbA1c) and a lipid profile for cholesterol.
- Pelvic Ultrasound: This imaging test allows the doctor to visualize your ovaries to look for the presence of cysts and to check the thickness of your uterine lining (endometrium).
Comprehensive Management: A Holistic Indian Approach
The most common question asked is, "How to cure PCOD permanently?" As of today, there is no permanent cure for this. However, it is an extremely manageable condition. The goal of PCOD treatment and PCOS management is to control symptoms, reduce long-term risks, and improve your quality of life. The best approach is a holistic one.
Navigating food choices with PCOD/PCOS can feel confusing, but it doesn't have to be. Let's simplify it by focusing on building your "PCOS Power Plate." This section provides a straightforward guide to the two most important categories of food: the nutrient-dense foods you should embrace to support your body, and the common hormone-disrupting foods you should limit. We'll give you practical swaps and tips that fit perfectly into an Indian lifestyle, making healthy eating a sustainable and effective part of your healing journey.
The Foundation: Indian Diet and Lifestyle Modification
This is the first, most powerful, and non-negotiable step. For many women with milder PCOD, this is often all that is needed.
- A Tailored Indian Diet Plan for PCOS: The goal is to combat insulin resistance. This approach is about nourishment, not deprivation. It means consciously choosing foods that work with your body to restore hormonal balance and vitality.
- Embrace Low Glycemic Index (GI) Foods: Switch from white rice to brown or red rice, and from fine wheat atta to whole wheat, jowar, bajra, and ragi. These release sugar into the blood slowly.
- Prioritize Fibre and Protein: Include plenty of dals, legumes (chana, rajma), sprouts, and non-starchy vegetables (leafy greens, beans, broccoli). Protein and fibre keep you full and help stabilize blood sugar.
- Incorporate Healthy Fats: Nuts, seeds (flax, chia), and avocados are excellent. Incorporate healthy traditional fats like pure desi ghee. In moderation, it provides essential fatty acids that support hormone production and aid in absorbing crucial vitamins like A, D, E, and K.
- Strictly Limit Sugar and Refined Carbs: This is crucial. Avoid sugary drinks, sweets, biscuits, maida-based products (white bread, pasta), and packaged foods.
- Mindful Eating: Connect with Your Food, Connect with Your Body: True nourishment goes beyond just what you eat; it's how you eat. Instead of rushing through meals, treat each one as a moment of self-care. Take the time to savour the flavours and textures of your food. This simple practice can dramatically improve digestion and help regulate the stress hormones that impact PCOS.
- Regular Physical Activity: Movement as Medicine: Find Joy in Being Active: The goal of 150 minutes of exercise per week might sound intimidating, but it's simply 30 minutes, five days a week. This isn't about punishing gym sessions.A brisk walk in your local park, climbing the stairs instead of taking the lift, a lively dance session to your favourite music at home, or a few rounds of Surya Namaskar can be incredibly effective.
- Cardio: Brisk walking, jogging, cycling, and swimming are excellent for improving insulin sensitivity.
- Strength Training: Building muscle helps your body use glucose more efficiently.
- Yoga: "Yoga offers a holistic approach to managing Polycystic Ovary Syndrome by addressing its root causes, particularly stress and hormonal imbalance. The practice works on multiple levels: it calms the nervous system to lower the production of the stress hormone cortisol, and it physically stimulates the endocrine glands. Specific asanas are recommended to improve pelvic health and support ovarian function. Consider incorporating these into your routine:
- Dhanurasana (Bow Pose): Helps alleviate menstrual discomfort and stimulates the reproductive organs.
- Baddha Konasana (Butterfly Pose): An excellent hip opener that improves blood flow to the pelvic region and can reduce stress.
- Surya Namaskar (Sun Salutation): A full-body workout that aids in weight management and improves overall hormonal balance.
Medical and Pharmaceutical Treatments
When lifestyle changes aren't enough, especially in PCOS, your doctor may recommend medication:
- Hormonal Contraceptives (Birth Control Pills): These are often prescribed to regulate menstrual cycles, reduce androgen levels, and clear up acne.
- Insulin-Sensitizing Drugs (Metformin): A medication traditionally for diabetes, Metformin is highly effective in treating insulin resistance in PCOS, which can help with weight loss and restore ovulation.
- Anti-Androgens: Drugs like Spironolactone can be used to combat symptoms like excess hair growth and acne specifically.
- Ovulation Induction Medications (Letrozole, Clomiphene): For women trying to conceive, these medications are used to stimulate the ovaries to release an egg.
Exploring Alternative Therapies in the Indian Context
Many Indian women seek alternative treatments. While promising, they should always be pursued under the guidance of qualified practitioners and in conjunction with your doctor's advice.
- Ayurveda for PCOS/PCOD: Ayurvedic approaches focus on balancing the doshas through herbal preparations (like Ashwagandha, Shatavari), detoxification therapies (Panchakarma), and specific dietary and lifestyle regimens.
- Indian Homeopathy for PCOS: Homeopathy offers constitutional remedies aimed at treating the individual as a whole to restore hormonal equilibrium.
Surgical Options (When Necessary)
In rare cases where medication and lifestyle changes fail, especially for infertility, a minimally invasive surgery called Laparoscopic Ovarian Drilling (LOD) may be considered
Fertility, Pregnancy, and Beyond
Can you get pregnant with PCOD or PCOS?
Absolutely. For women with PCOD, pregnancy can often be achieved with lifestyle management. For women with PCOS, it can be more challenging due to lack of ovulation, but it is very possible with medical help. Infertility treatments have a high success rate.
It's vital to work with your gynaecologist before and during pregnancy, as PCOS increases the risk of complications like gestational diabetes, pre-eclampsia (high blood pressure), and premature birth.
PCOD and PCOS Treatment at Baluni Hospital, Dehradun, India
For those seeking expert care in Uttarakhand, Baluni Hospital stands out as a leading centre for treating PCOD and PCOS problems in Dehradun. With a patient-centric approach and modern facilities, the hospital offers a comprehensive pathway to managing these complex conditions.
Led by a team that includes some of the best gynecologists in Dehradun, Baluni Hospital provides personalized diagnosis and treatment protocols tailored to each woman's unique needs. The hospital is equipped with advanced diagnostic tools and utilizes modern infertility treatment solutions to help women on their journey to conception and motherhood.
Recognizing that PCOD/PCOS requires holistic care, the expert gynecologists often work in collaboration with endocrinologists for long-term symptom management. Furthermore, patients have access to dedicated counsellors for guidance on critical lifestyle and diet modifications.
To ensure your consultation is as productive as possible, you should come prepared with detailed information regarding your:
- Medical history
- Current symptoms and their duration
- Past treatment history
- Family history of hormonal issues or diabetes
- Any previous medical reports or test results
Conclusion: Taking Charge of Your Hormonal Health
Navigating the world of PCOD vs PCOS in India can feel overwhelming, but clarity is the first step toward empowerment. Remember this: PCOD is a common condition, and PCOS is a more complex syndrome, but both are curable.
Your health journey is unique. It requires a partnership between you and your healthcare team, built on a foundation of proactive lifestyle choices. By adopting a balanced Indian diet, engaging in an active lifestyle, and receiving consistent medical guidance, you can effectively manage your symptoms, mitigate long-term health risks, and lead a full, vibrant, and healthy life.
Don't let confusion or fear hold you back. If any part of this guide resonates with you, take the next step. Schedule a consultation with a gynaecologist, ask questions, and start building your personalized roadmap to wellness today.
Frequently Asked Questions (FAQs)
Q1: What is the main difference between PCOD and PCOS?
A: The main difference is severity and impact. PCOD is a condition primarily affecting the ovaries and is often manageable with lifestyle changes. PCOS is a more serious metabolic syndrome that affects the entire body, is strongly linked to insulin resistance, and carries long-term health risks like diabetes and heart disease.
Q2: Can PCOD turn into PCOS?
A: While PCOD is not thought to "turn into" PCOS, an unmanaged PCOD condition, especially with continued weight gain and poor lifestyle, can worsen over time. The symptoms can become more severe and start to resemble PCOS, developing metabolic issues like insulin resistance. Early management is key to preventing this progression.
Q3: Which is more serious, PCOD or PCOS?
A: PCOS is considered more serious due to its systemic nature and the associated long-term health risks, including a higher likelihood of developing type 2 diabetes, high blood pressure, cardiovascular disease, and endometrial cancer.
Q4: Can you get pregnant with PCOD or PCOS?
A: Yes. For many women with PCOD, pregnancy is achievable with lifestyle modifications. For women with PCOS, it can be more challenging due to irregular ovulation, but fertility treatments are highly effective. It is crucial to consult a gynaecologist for a pre-conception plan.
Q5: How to treat PCOS naturally in India?
A: "Natural" treatment for PCOS revolves around an intensive lifestyle overhaul. This includes adopting a traditional, low-glycemic Indian diet (rich in millets, dals, and vegetables), eliminating sugar and processed foods, engaging in regular exercise like yoga and strength training, managing stress through meditation, and ensuring adequate sleep. Ayurvedic and homeopathic remedies, under the guidance of qualified practitioners, are also popular natural approaches.
Q6: Is PCOD common in Indian women?
A: Yes, it is extremely common. Studies estimate that up to 20%, or 1 in 5, women in India suffer from PCOD, making it one of the most prevalent endocrine issues in the country.
Q7: How does PCOS impact mental health?
A: PCOS has a significant impact on mental health. The hormonal imbalances can directly contribute to mood swings, anxiety, and depression. Furthermore, dealing with visible symptoms like weight gain, acne, and hair loss can severely affect self-esteem and body image. Seeking mental health support is a crucial part of holistic PCOS management.
Q8: Can lifestyle changes alone effectively manage PCOS?
A: In some mild cases of PCOS, dedicated and consistent lifestyle changes can manage symptoms very well. However, because PCOS is a complex metabolic syndrome, most women require a combination of aggressive lifestyle management and medical support (like Metformin or hormonal treatments) to control symptoms and prevent long-term complications.







